The In Silico Science team analyzed 25 studies comprising 1810 smokers on the possible cardiovascular effects of cigarette substitution: the findings gave no indications that e-cigarette use is more harmful than smoking. Moreover, switching may lead to some possible health benefit
Catania – January 11, 2023 – The substitution of electronic cigarettes for combustible cigarettes in public health programs is a choice already taken by some countries: but there is still concern regarding some possible negative health outcomes of nicotine delivery systems.
In Silico Science is a project lead by CoEHAR, Center of Excellence for the acceleration of Harm Reduction, which aims to analyze the available scientific literature to data about the possible health effects of e-cigarettes. Moreover, authors evaluated the studies for methodological biases and reporting issues as well as rate the strength of the evidence.
The latest review conducted by Dr. Renée O’Leary, CoEHAR researcher and one of the leading experts in the field of systematic reviews, analyzed evidence from clinical research on human participants to address the question: “What are the cardiovascular health effects resulting from the substitution of e-cigs for conventional cigarettes?”.
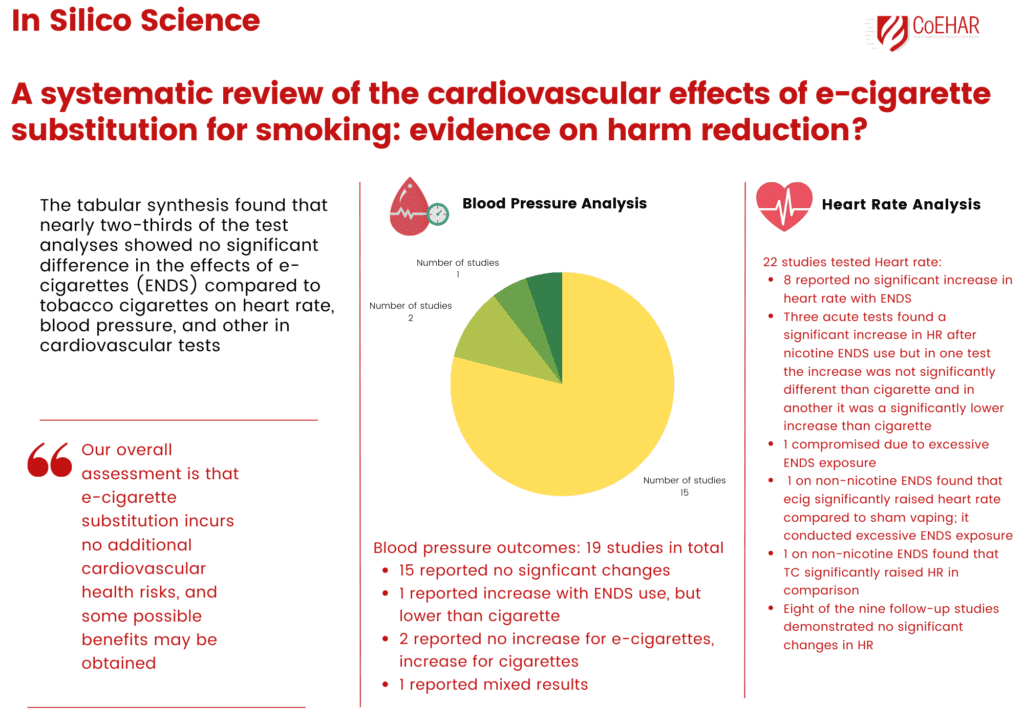
The research covered 25 studies comprising 1,810 participants who smoked. The authors found that nearly two thirds of the tests analyzed showed e-cigarettes do not bring any additional harm to a smoker’s health, specifically in relation to heart rate, blood pressure and cardiovascular test. In fact, researchers evaluated evidence from two clinical studies that showed that the use of e-cigarettes could lead to a potential benefit. For example, participants with hypertension experienced a clinically significant reduction in systolic blood pressure after one year of electronic nicotine delivery systems use.
Regarding methodological limitations and flaws, twenty studies were rated at high risk of bias, and five as some concerns. Among the most common methodological issues, the review highlighted that seven studies are rated with a risk for ascertainment bias with participants of only one gender, young adult participants, or exceptionally light or heavy patterns of tobacco cigarette consumption.
The author emphasizes the small sample size in half of the studies reduces the confidence in their findings. Some studies had vaping protocols that did not replicate how individuals use e-cigarettes in practice.
“Our review provides a detailed and up-to-date body of data regarding the possible implications for human health that comes from e-cig substitution” stated Dr. O’Leary, first author of the study. “Data from the review support the idea that the use of e-cigarettes led to no additional cardiovascular heart risk and smokers who choose to switch can benefit from this choice. However, as emerged in other reviews, we observed some methodological issue and flaws, mainly due to the design of the studies that do not represent real e-cig use and the limitations such as participants sample size or lack reporting of previous smoking history”.
THE STUDY
The review conducted by the In Silico Science team covered 25 studies from January 31, 2021, to April 29, 2021. To be considered for the review, a study was required to have either a comparator group who smoked combustible tobacco (cigarettes) or a within subject testing of participants who had substituted electronic nicotine delivery systems for smoking. Moreover, the study had to report outcome data or analysis from cardiovascular tests.
The studies were conducted in the USA (8), UK (6), Italy (4), Germany (2), and one each in Belgium, Greece, Indonesia, Poland, and South Africa. The participants ranged in age from 18 to 65 comprising 1,810 participants who smoked.
Fourteen studies conducted acute testing; eleven studies presented follow-up data ranging from 5 days to 24 months. Regarding possible effects of vaping on heart rate, eight acute studies found no significant increase in heart rate with electronic nicotine delivery system use. Three acute tests found a significant increase in heart rate after nicotine e-cigarette use, but in one test the increase was not significantly different than tobacco cigarette and in another it was a significantly lower increase than tobacco cigarette. Eight of the nine follow-up studies demonstrated no significant changes in heart rate.
There were 19 studies that tested blood pressure, eight acute studies and 11 follow-up studies. Fifteen studies indicated no significant changes. Two studies showed that tobacco cigarette use significantly increased blood pressure while electronic nicotine delivery system use did not. Only one study compared dual users with exclusive e-cig users, finding that exclusive users had significantly better improvements in heart rate and blood pressure than dual users.
Seven studies were rated with a risk for ascertainment bias with participants of only one gender, young adult participants, or exceptionally light or heavy patterns of tobacco cigarette consumption. For studies on cardiovascular functioning, the age of participants is a serious issue for ascertainment bias. Another methodological issue contributing to the low certainty in the evidence is sample sizes of the studies. Eleven studies were conducted with 20 electronic nicotine delivery systems participants or less.
Moreover, different models of e-cigarettes were used across the studies: findings based on the first e-cig models may not be applicable to current ones. Some studies do not consider previous smoking history. Finally, some researchers use vaping protocols that do not replicate users’ e-cig experience in practice.
Authors urge researchers to pay close attention to their research designs: more quality evidence is certainly needed to inform if e-cigarette substitution is a worthwhile treatment option for harm reduction for persons who smoke.




